Now, more than ever, staying up to date on the latest trends and innovations in ultrasound is essential for physicians. This year, the annual meeting of the American Institute of Ultrasound in Medicine (AIUM) is being transformed into UltraCon! This new conference puts you at the center of the conversation where expertise meets interaction and debate. So how can you ensure that you are prepared to take full advantage of this transformative opportunity?
In a previous post, we highlighted how you could explore new, exciting, and current technologies in ultrasound; identify the different approaches to diagnostic ultrasound; and determine which ultrasound techniques can help you advance your practice at “Can You Do That With Ultrasound?” on day one at UltraCon (March 25–29, 2023). Day two at UltraCon offers attendees more opportunities to deepen their understanding of ultrasound—both as a diagnostic tool and in treating injuries and diseases—through two additional symposiums: “Optimizing Ultrasound Image Quality” and “Ultrasound Diagnoses You Can’t Miss.”
Optimizing Ultrasound Image Quality
Optimizing ultrasound image quality and, ultimately, patient care is at the heart of this symposium. As a healthcare professional, you will be well-equipped to succeed at this task with knowledge gained through key topics such as physics, knobology, and Doppler, as well as improving patient/probe position. You will benefit from roundtable discussions that cover image reviews and quality assurance—useful topics that can help move one step closer to improving patient outcomes. Earn 5 CMEs for learning about ultrasound technology advancements, advancing your image acquisition techniques, and finding ways to improve image quality. This symposium is sure to contribute to providing better patient care!
This symposium will feature a total of 8 engaging and interactive sessions for attendees to participate through in groups:
- “Physics: So Easy it Hertz,” led by Frederick Kremkau, PhD, FAIUM. How does ultrasound work? It’s all about physics. Knowing the role physics plays will help you avoid artifacts.
- “Know Your Knobs,” led by Elena S. Sinkovskaya, MD, PhD. To even get an ultrasound image, you must know how your machine works, how to make fundamental adjustments, and how to make optimal use of B-mode. Glossary handout included.
- “Elements of Scanning,” led by Margaret R. Lewis, MD. Improve your ultrasound diagnostics by understanding optimal patient and transducer positioning techniques, equipment quality assurance, and more.
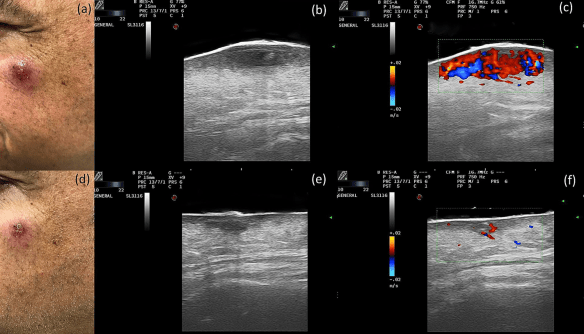
- “Demystifying Doppler,” led by Tracy Anton, MD. What is Doppler ultrasound? How does it work? How do I select the correct equipment? How do I interpret the results? Learn all this and more by attending.
- “Just Images Roundtable,” led by Mishella Perez, BS, RDMS, RDCS, FAIUM, and Yvette S. Groszmann, MD, MPH. Learn what you can do to improve image quality across specialties, including OB, GYN, MSK, POCUS, and Vascular.
- “Echoes of the Past to the Voices of the Future,” led by Frederick Kremkau, PhD, FAIUM. Attend this session to understand how prior advancements in ultrasound technology have established the scaffold for the possibilities of the use of diagnostic ultrasound in the present and the future.
- “Ultrasound Quality Assurance Roundtable,” led by Timothy Canavan, MD, MSc, FAIUM, Therese Cooper, BS, RDMS, David Jones, MD, FAIUM, Anita Moon-Grady, MD, and Aubrey Rybyinski, MD. Understanding the role of accreditation and continuous QA is essential to ensuring the best outcomes for patients. Hear from a panel of experts to better guide your practice and get answers to your questions.
- Image Quality Trivia: Test your ultrasound knowledge during this fun, quiz-style game where the entire audience participates. Topics include OB, fetal echo, GYN, physics, MSK, and general imaging.
Ultrasound Diagnoses You Can’t Miss
Ultrasound diagnoses are a crucial part of maintaining top-level medical care. Ultrasound experts from various disciplines meet in this symposium to share their expert knowledge and experience, allowing participants to stay on top of the imaging findings and avoid any form of misdiagnosis. During the symposium, a multispecialty expert panel will create an interactive discussion for the attendees to apply their learning to real clinical scenarios. And what’s more? You can earn up to 5.75 CMEs just by attending this “Ultrasound Diagnoses You Can’t Miss” symposium!
This symposium will feature a total of 17 engaging and interactive sessions for attendees to participate in where subspecialty discussion, breakout opportunities, and rapid case reviews will take place.
UltraCon is an incredible opportunity for medical ultrasound practitioners who want to stay up-to-date on all things related to medical ultrasound technology. From interactive debates to resource handouts, exhibitor sandboxes, and focus groups—this event has something for everyone! Come prepared with an open mind and get ready to connect with experts from around the world while learning about the exciting new possibilities that are transforming the field of medical ultrasound today! Don’t miss out—All of this is just what is available on the second day of symposia at UltraCon. Check out the Full Schedule to get a sneak peek at everything you could learn.
Arian Tyler, BS, is the Digital Media and Communications Coordinator for the American Institute of Ultrasound in Medicine (AIUM).